Microglia research has emerged as a pivotal field in neuroscience, shedding light on the vital roles these cells play in the brain’s immune system. These specialized glial cells not only patrol the brain for signs of damage but also engage in the critical process of synaptic pruning, influencing communication between neurons. Recent studies indicate that dysregulation of microglial functions could contribute to the onset of Alzheimer’s disease and other neurodegenerative disorders. Under the leadership of prominent researchers like Beth Stevens, groundbreaking work is uncovering how microglial cells may offer innovative pathways for biomarker identification and therapeutic development. As we continue to explore the complexities of microglia, the potential for advancing treatments that improve the lives of millions affected by Alzheimer’s disease becomes increasingly apparent.
The research focusing on glial cells, particularly microglia, is transforming our understanding of how the brain maintains its health and responds to injury. These immune cells act as guardians of the central nervous system, clearing cellular debris and managing synaptic connections essential for brain function. Investigations into their mechanisms have revealed critical links to neurodegenerative diseases, highlighting synaptic pruning as a vital process that can malfunction in conditions like Alzheimer’s disease. With experts such as Beth Stevens leading the charge, this area of study promises to unveil new insights and therapeutic options tailored to combat such debilitating disorders. As the brain’s immune agents, microglia are crucial players in the ongoing battle against cognitive decline.
The Role of Microglia in Alzheimer’s Disease
Microglia are specialized cells in the brain that serve as the primary immune defense. They continuously monitor and respond to changes in the environment, playing a crucial role in maintaining brain health. In the context of Alzheimer’s disease, microglia can either help or hinder the progression of the disease. Studies have suggested that an imbalance in microglial activity—particularly in the process of synaptic pruning—may lead to the degeneration of neurons, a hallmark of Alzheimer’s. Understanding how these mechanisms work could reveal novel therapeutic strategies for combating this neurodegenerative disorder.
Research led by Beth Stevens has illustrated how microglial dysfunction can exacerbate conditions such as Alzheimer’s disease. When microglia incorrectly prune synapses, they can disrupt neural networks and contribute to cognitive decline. Stevens emphasizes the importance of investigating these cellular processes to better understand the complex interactions within the brain’s immune system. By uncovering the intricacies of microglial behavior, researchers hope to develop interventions that can restore proper synaptic function and potentially halt disease progression.
Investigating Neurodegenerative Disorders through Synaptic Pruning
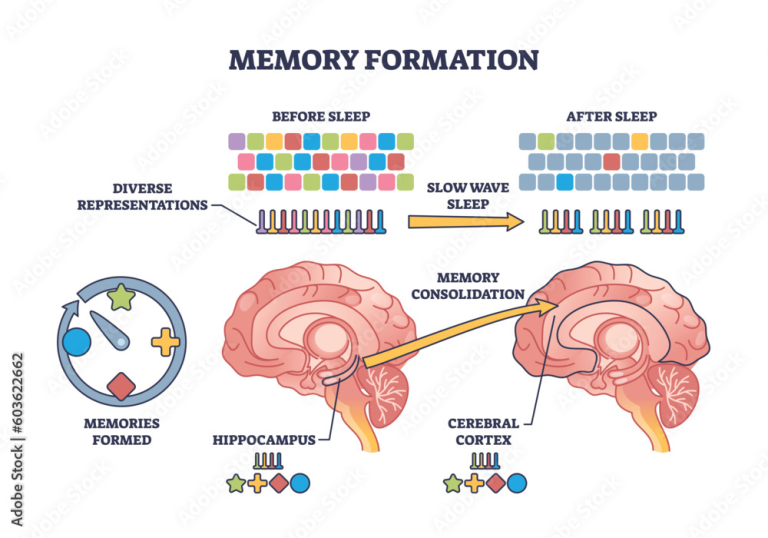
Neurodegenerative disorders like Alzheimer’s and Huntington’s disease are characterized by the progressive degeneration of the nervous system, leading to cognitive and motor decline. One area of ongoing research is the process of synaptic pruning, which is essential for the normal development and functioning of neural circuits. In healthy brains, microglia facilitate this pruning at appropriate levels. However, when the balance is disrupted, excessive pruning can lead to significant losses of synaptic connections, directly impacting cognitive functions.
Beth Stevens and her team have focused extensively on the relationship between synaptic pruning and neurodegenerative disorders. Their findings suggest that targeted modulation of microglial activity could provide a pathway for therapeutic interventions. By developing biomarkers to identify synaptic dysfunction early, researchers aim to create novel approaches that could slow down or even prevent the onset of neurodegenerative diseases. This line of inquiry could reshape treatment paradigms, leading to better outcomes for millions affected by such conditions.
The Importance of Curiosity-Driven Research in Neuroscience
Curiosity-driven research serves as the backbone for significant breakthroughs in neuroscience. As Beth Stevens recalls, her journey began with a fundamental interest in the brain’s immune system and its role in synaptic development. It is through this lens that Stevens has made her mark, illustrating how foundational inquiry can yield unexpected insights into complex neurodegenerative diseases such as Alzheimer’s. The willingness to explore unknown territories often results in groundbreaking discoveries that have the potential to change the landscape of medical research.
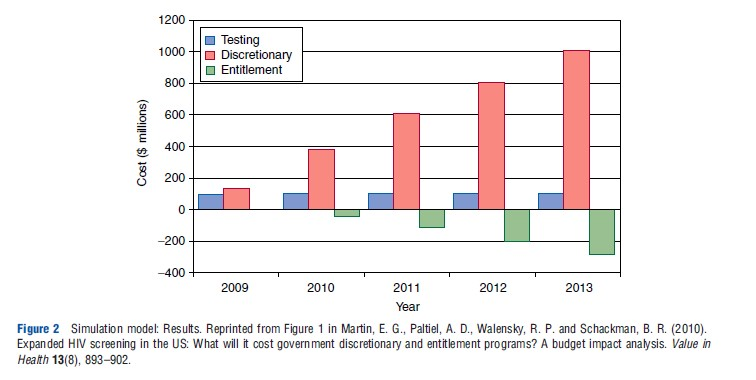
Funding from agencies like the National Institutes of Health has been pivotal in supporting this exploratory research. The long-term benefits of investing in curiosity-driven studies can lead to advancements that translate into clinical practices, offering hope to patients suffering from neurodegenerative disorders. By encouraging a culture of inquiry and innovation, the scientific community can continue to unravel the mysteries of the brain and develop effective treatments for devastating conditions like Alzheimer’s disease.
Beth Stevens: A Pioneer in Microglial Research
Beth Stevens is at the forefront of microglial research, being recognized for her innovative contributions to our understanding of how these brain immune cells function. Her work has not only illuminated the role of microglia in maintaining neural health but has also provided insights into their involvement in neurodegenerative diseases such as Alzheimer’s. Stevens’ dedication to uncovering the underlying mechanisms of microglial activity exemplifies how curiosity can drive impactful scientific advancements.
Receiving accolades such as the MacArthur Fellowship highlights the importance of her contributions to neuroscience. Stevens’ research sheds light on the potential of harnessing microglial functions to mitigate the progression of Alzheimer’s disease. By transforming our understanding of these cells, she paves the way for new therapeutic strategies that target the brain’s immune system, offering renewed hope for patients affected by neurodegenerative disorders.
Exploring the Synaptic Landscape in Alzheimer’s Research
The synaptic landscape of the brain is intricately linked to cognitive function and overall brain health. In Alzheimer’s disease, alterations in synaptic density and connectivity can lead to significant functional impairments. Research on synaptic pruning by microglia is crucial for understanding the shifts in synaptic architecture associated with Alzheimer’s. By elucidating the links between synaptic health and disease, scientists can identify potential targets for therapeutic intervention.
Recent advancements in imaging techniques and molecular biology have allowed researchers to study synaptic changes at unprecedented levels of detail. Stevens’ lab has employed these methods to observe how microglial-mediated pruning affects neural circuits. Insights from this research could inform the development of strategies aimed at preserving synaptic integrity, which is essential for maintaining cognitive functions in Alzheimer patients.
Future Directions in Microglial Research
The future of microglial research looks promising, with new technologies paving the way for deeper investigations into their roles in the brain. Studies are increasingly focusing on how microglia interact with neurons and other cell types in various neurodegenerative disorders. Understanding these interactions is critical for developing targeted therapies that can modulate microglial function and restore balance in the brain’s immune system.
As researchers like Beth Stevens continue to explore these complex cellular interactions, they are likely to uncover new biomarkers and therapeutic targets. This direction not only broadens our understanding of Alzheimer’s disease but also holds potential for treating other neurodegenerative conditions. The ongoing exploration of microglial biology may unlock novel strategies that enhance brain resilience and improve the quality of life for millions worldwide.
Microglia: The Brain’s Immune Guardians
Microglia play a vital role as the primary immune defenders of the brain, constantly surveilling for injury, infection, or diseased cells. These cells are essential for maintaining overall brain health by clearing debris and modulating inflammation. However, their role becomes more complex when studying neurodegenerative disorders like Alzheimer’s disease, where microglial activity can become maladaptive and contribute to pathology.
Understanding the dual nature of microglia—both protective and potentially harmful—is crucial for developing effective interventions. Researchers are investigating ways to enhance the beneficial functions of microglia while inhibiting their harmful actions. This insight into microglial behavior not only informs our understanding of Alzheimer’s disease but also has implications for the treatment of a range of neurodegenerative disorders.
Synaptic Pruning and Its Implications for Neurodegeneration
Synaptic pruning, a process that optimizes neural connections, is essential for healthy brain development and function. However, in Alzheimer’s disease, the pruning process can become dysregulated, leading to the loss of synapses critical for cognitive function. Beth Stevens’ research underscores the importance of understanding how synaptic pruning contributes to neurodegenerative processes, with implications for developing new therapeutic approaches.
By investigating the mechanisms behind abnormal synaptic pruning, researchers aspire to create treatments that can halt or reverse cognitive decline in diseases like Alzheimer’s. This has profound consequences not only for the understanding of neurodegeneration but also for the development of strategies that enhance synaptic health and overall brain function throughout one’s life.
Innovative Therapies Emerging from Microglial Research
As the understanding of microglia advances, innovative therapies targeting these cells are emerging. By modulating the activity of microglia, researchers aim to restore their protective functions while mitigating their detrimental effects in neurodegenerative diseases like Alzheimer’s. Therapies designed to enhance microglial function could provide new avenues to combat cognitive decline and preserve neuronal health.
The potential for targeted microglial therapies extends beyond Alzheimer’s to other neurodegenerative conditions. As the research progresses, the hope is to develop precision medicine approaches that tailor interventions based on individual patient profiles. This shift could redefine treatment paradigms, moving toward more personalized and effective strategies for neurodegenerative diseases.
Frequently Asked Questions
What role do microglia play in Alzheimer’s disease research?
Microglia are crucial components in Alzheimer’s disease research as they act as the brain’s immune system. They help clear away dead or damaged cells and engage in synaptic pruning, processes that can become dysregulated in Alzheimer’s, contributing to neurodegeneration. Understanding their behavior provides insights into potential treatment avenues for this condition.
How does synaptic pruning by microglia affect neurodegenerative disorders?
Synaptic pruning by microglia is essential for healthy brain function, but improper pruning is linked to neurodegenerative disorders, including Alzheimer’s disease. Research has shown that excessive or insufficient pruning can disrupt neuronal communication and lead to cognitive decline, making it a vital focus for developing therapies against these diseases.
What discoveries have been made by Beth Stevens regarding microglia and Alzheimer’s?
Beth Stevens has discovered that microglial cells play a significant role in both the maintenance and destruction of neural connections, influencing the progression of Alzheimer’s disease. Her research has revealed that improper synaptic pruning by microglia can lead to neuronal loss, highlighting the need for further study into treatments that can modulate microglial activity.
How is microglial research advancing treatments for neurodegenerative diseases?
Microglial research is advancing treatments for neurodegenerative diseases by identifying biomarkers and understanding the processes of synaptic pruning and inflammation in the brain. Studies like those led by Beth Stevens are paving the way for new therapeutic strategies aimed at restoring normal microglial function, thereby improving outcomes for conditions like Alzheimer’s.
What impact does microglial dysfunction have on the brain’s immune system?
Dysfunction of microglia can severely compromise the brain’s immune system, leading to heightened inflammation and impaired synaptic pruning. This dysfunction is associated with various neurodegenerative diseases, including Alzheimer’s disease, as it disrupts the balance needed for maintaining neural health and function.
Why is basic microglia research important for understanding Alzheimer’s disease?
Basic microglia research is critical for understanding Alzheimer’s disease because it lays the groundwork for identifying the cellular and molecular mechanisms driving disease progression. This foundational knowledge helps to generate hypotheses that can lead to innovative treatment strategies targeting microglial behavior, which Stevens and others are actively pursuing.
| Key Points | Details |
|---|---|
| Microglia’s Role | Microglia act as the brain’s immune system, clearing dead cells and pruning synapses. |
| Impact on Alzheimer’s | Improper pruning by microglia can contribute to Alzheimer’s and other neurodegenerative conditions. |
| Research Foundation | Research is supported by NIH funding and curiosity-driven science. |
| Future of Treatments | New biomarkers and therapies are being developed to mitigate Alzheimer’s disease. |
| Broader Implications | Microglial research allows for breakthroughs in understanding and treating human diseases. |
Summary
Microglia research is crucial in understanding the brain’s immune response and its implications for neurodegenerative diseases such as Alzheimer’s. Investigators like Beth Stevens have highlighted the transformative role of microglial cells in disease processes, revealing that their improper functioning can lead to severe conditions. Ongoing studies not only shed light on the underlying mechanisms of these diseases but also pave the way for developing innovative treatment options, thereby enhancing the quality of life for millions affected by Alzheimer’s. The continuous funding and support for basic science research remain vital to uncovering the complexities of the brain and finding potential solutions.